UNDERSTANDING CHOLANGIOCARCINOMA
Cholangiocarcinoma, pronounced (koh-LAN-jee-oh-KAR-sih-NOH-muh), is a rare bile duct cancer of the liver.
MORE INFORMATION
With approximately 10,000 cases a year being diagnosed in the United States, cholangiocarcinoma is the second most common primary liver cancer in the world. We’ve provided resources to help.

CCF offers both an infographic and physician tear off to help you navigate your journey.
Click below to download each PDF.

Overview
What is cholangiocarcinoma?
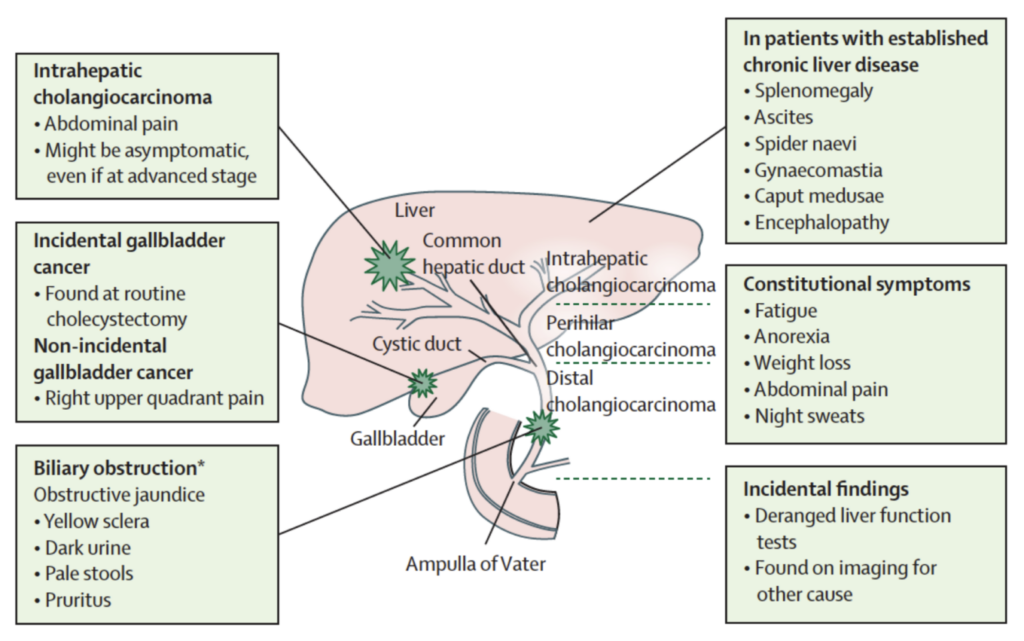
Cholangiocarcinoma starts in the bile duct, a thin tube, about 4 to 5 inches long, that reaches from the liver to the small intestine. The major function of the bile duct is to move a fluid called bile from the liver and gallbladder to the small intestine, where it helps digest the fats in food.
Different parts of the bile duct system have different names. In the liver it begins as many tiny tubes (ductules) where bile collects from the liver cells. The ductules come together to form small ducts, which then merge into larger ducts and eventually the left and right hepatic ducts. The ducts within the liver are called intrahepatic bile ducts. These ducts exit from the liver and join to form the common hepatic duct at the hilum.
About one-third of the way along the length of the bile duct, the gallbladder (a small organ that stores bile) attaches by a small duct called the cystic duct. The combined duct is called the common bile duct. The common bile duct passes through part of the pancreas before it empties into the first part of the small intestine (the duodenum), next to where the pancreatic duct also enters the small intestine.
Cancers can develop in any part of the bile duct and, based on their location, are classified into 3 types:
- Intrahepatic cholangiocarcinoma
- Perihilar cholangiocarcinoma
- Distal cholangiocarcinoma

Key Statistics
Key Statistics
- About 10,000 people in the United States develop cholangiocarcinoma each year.
- Cholangiocarcinoma is much more common in Asia, mostly because of a common parasitic infection of the bile duct.
- Almost 2 out of 3 people with cholangiocarcinoma are 65 or older when it is found.
- The average age of people diagnosed with cancer of the intrahepatic bile ducts is 70.
- The average age of people diagnosed with cancer of the extrahepatic bile ducts (perihilar or distal cholangiocarcinoma) is 72.
- The chances of survival for patients with bile duct cancer depend to a large extent on its location and how advanced it is when it is found. It also may depend on access to innovative treatments such as clinical trials. Clinical trials offer access to therapies that may not be available through standard care, potentially providing patients with more effective options to combat the disease.
Adapted from the American Cancer Society
About Rare Cancers
Why is cholangiocarcinoma considered a rare cancer?
Rare cancers are those that affect fewer than 40,000 people per year in the U.S. As a group, they make up just over a quarter of all cancers.
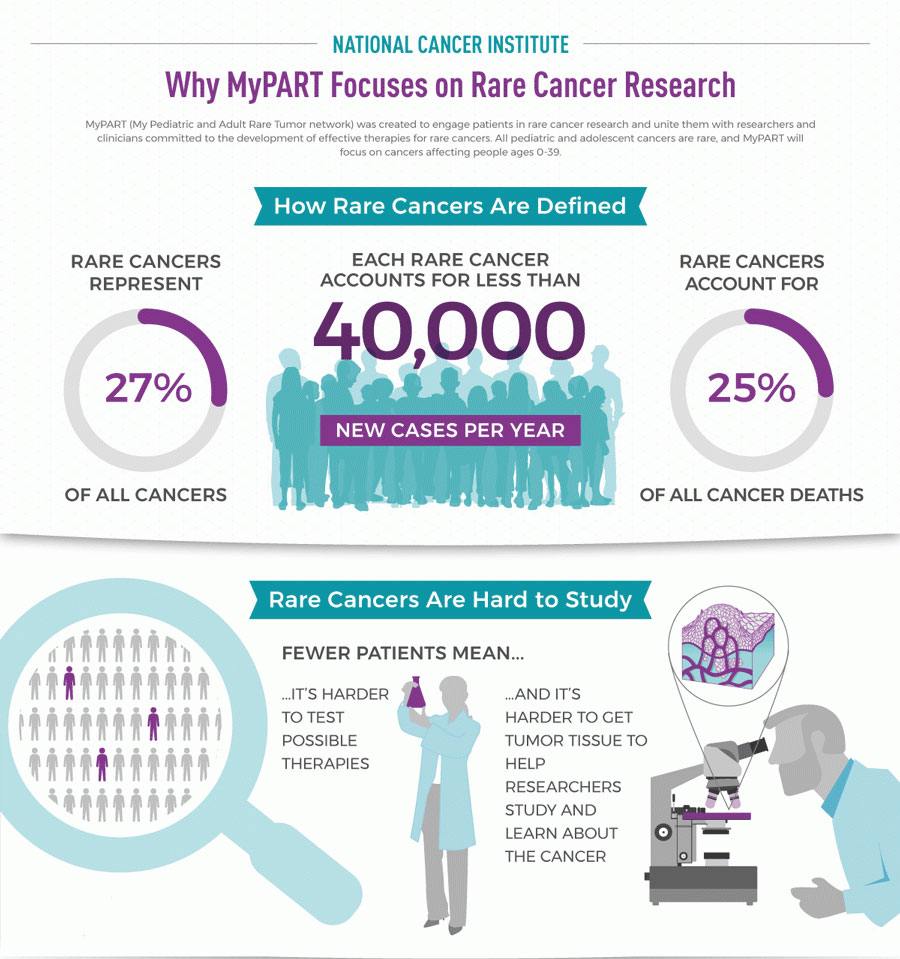
Rare cancers are challenging for patients, doctors, and scientists.
For patients:
- It often takes a long time from the time you think something is wrong to the time when doctors know that you have a rare cancer and what kind of cancer it is.
- It is hard to find doctors who know a lot about your cancer and how to treat it.
- It is hard to know what to do when doctors don’t agree on how to treat your cancer.
- You may need to travel far from your home and family to get treatment for your rare cancer.
For doctors:
- You may not know what to tell your patient about what to expect with their rare cancer.
- You may not have been trained in how to treat this type of rare cancer.
- It is hard to find an expert in the rare cancer who can answer questions or to whom you can refer your patient.
For scientists:
- There may be no information about the rare cancer to give you ideas on which drugs could treat it.
- There may be no animal or cell models of the rare cancer in which to test your ideas.
- There may not be enough tumor samples from rare cancer patients available for your research.
- If you have an idea of a drug that could treat the cancer, it may be hard to find enough patients with the rare cancer to test your idea.
Adapted from cancer.gov

Risk Factors
DISEASES IN THE LIVER OR BILE DUCTS:
OTHER RISK FACTORS INCLUDE:
Adapted from National Institutes of Health: http://www.cancer.gov/
Symptoms
- Chills
- Clay-colored stools
- Dark urine
- Fatigue
- Itching (pruritus)
- Loss of appetite
- Nausea
- Pain in the upper right abdomen that may radiate to the back
- Weight Loss
- Yellowing of the skin (jaundice)
Cancer in different areas may cause different symptoms.

Staging
After a person is diagnosed, doctors will try to figure out if it has spread, and if so, how far. This process is called staging. The stage of a cancer describes how much cancer is in the body. It helps determine how serious the cancer is and how best to treat it. Doctors also use a cancer’s stage when talking about survival statistics.
Although each person’s cancer experience is unique, cancers with similar stages tend to have a similar outlook and are often treated in much the same way.
How is the stage determined?
The staging system most often used is the American Joint Committee on Cancer (AJCC) TNM system, which is based on 3 key pieces of information:
- The extent (size) of the main tumor (T): How large has the cancer grown? Has the cancer reached nearby structures or organs?
- The spread to nearby lymph nodes (N): Has the cancer spread to nearby lymph nodes?
- The spread (metastasis) to distant sites (M): Has the cancer spread to distant lymph nodes or distant organs such as the bones, lungs, or peritoneum (the lining of the abdomen )?
Numbers or letters after T, N, and M provide more details about each of these factors. Higher numbers mean the cancer is more advanced.
Once a person’s T, N, and M categories have been determined, this information is combined in a process called stage grouping to assign an overall stage. For more on this, see Cancer Staging.
Cancer staging can be complex, so ask your doctor to explain it to you in a way you understand.