Treatment options
You are your own best advocate.
The Cholangiocarcinoma Foundation strongly recommends that you discuss your treatment goals with your healthcare team and know all of your options at every stage of your disease.
Choosing Your Healthcare Team
Learn about the importance of seeing an oncologist and surgeon who specialize in cholangiocarcinoma.

Surgery for cholangiocarcinoma is a complex operation that depend on tumor location and extension (if the tumor has grown through the layers of the tissue in which it started) and should be done by an experienced surgeon working at a major medical center whenever possible. There are 2 general types of surgical treatment for cholangiocarcinoma — potentially curative surgery and palliative surgery.
A. Potentially curative surgery
This is used when imaging tests indicate a good chance that the surgeon may be able to remove all of the cancer. Doctors may use the term resectable to describe cancers they believe can be removed completely (by potentially curative surgery) and unresectable to describe those they think have spread too far or are in too difficult a place to be entirely removed by surgery. Unfortunately, only a small portion of bile duct cancers are resectable at the time they are first found.
For resectable cancers, the type of operation depends on the cancer location
- Intrahepatic cholangiocarcinoma: These cancers are in the bile ducts within the liver. To treat these cancers, the surgeon cuts out the part of the liver containing the cancer.
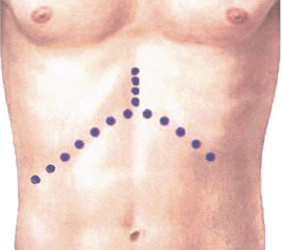
- The open surgical approach is often through an incision beneath the ribcage like the one shown on the right. Some tumors can be removed through smaller incisions with the help of a camera and special long instruments. This is called a laparoscopic liver resection. It is a complicated operation and requires an experienced team of surgeons and assistants. Your liver surgeon will discuss with you the best approach appropriate for removing your tumor(s).
- Removing small tumors on the edge is called a liver wedge resection
- However, most tumors require a bigger surgery to resect the tumor(s) completely. Removing part of the liver is called a partial hepatectomy. Sometimes this means that a whole lobe (section) of the liver must be removed. This is called hepatic lobectomy. Depending on how healthy your liver is before the surgery, about 60 -80% of the liver can be removed safely. Your liver will begin to grow back within days after your operation, and in six weeks will be just about the same volume it was before your surgery.
- Perihilar cholangiocarcinoma (bile duct cancer): These cancers begin where the branches of the bile duct first leave the liver. Surgery for these cancers requires great skill, as the operation is quite extensive. Usually, part of the liver is removed, along with the bile duct, gallbladder, nearby lymph nodes, and sometimes part of the pancreas and small intestine. Then the surgeon connects the remaining ducts to the small intestine. This is not an easy operation for the patient, and there can be surgical complications.
- Distal cholangiocarcinoma (bile duct cancer): These cancers are further down the bile duct near the pancreas and small intestine. If you had distal cholangiocarcinoma, you may be a candidate for Whipple surgery, a procedure in which your cancer surgeon will remove the entire head of the pancreas, the gallbladder, part of the stomach, part of the small intestine, and the bile duct, followed by a complex reconstruction where your remaining stomach, pancreas and bile duct are all reconnected to your small intestine. This is a complex procedure that requires a specialized surgical team.
Many pancreas operations require an open incision. This incision can be beneath the ribcage like the one shown in blue, or it can be vertical, like the one shown in red. Some tumors can be removed through smaller incisions with the help of a camera and special long instruments. This is called a laparoscopic pancreatectomy. Your surgeon will determine which approach is most appropriate for you. - Possible risks and side effects: The risks and side effects of surgery depend in large part on the extent of the operation and a person’s general health. All surgery carries some risk, including the possibility of bleeding, infections, complications from anesthesia, pneumonia, and even death in rare cases. People will have some pain from the incision for some time after the operation, but this can usually be controlled with medicine. Surgery for bile duct cancer is a major operation that might mean removing parts of several organs. This can significantly affect a person’s recovery and health after the surgery, because most of the organs involved in digestion, eating and nutrition problems are often long-term side effects of surgery for this cancer.
Liver transplantation for unresectable cancers: The American Association for the Study of Liver disease Guidelines recommends that potential transplant candidates should be expeditiously referred to major cancer centers that have established protocols for oncologic assessment and treatment approved by United Network for Organ Sharing (UNOS).
For some people with early stage unresectable intrahepatic or perihilar bile duct cancers, removing the liver and bile ducts and then transplanting a donor liver may be an option. In some cases, it might even cure the cancer.
For those who are eligible for a transplant there are some obstacles including:
- Not many centers accept patients with bile duct cancer into their transplant programs.
- Few livers are available for patients with cancer because they are generally used for more curable diseases.
- Waiting until a liver is available can take a long for some people.
To overcome these obstacles, patients have two options:
- One option is having a living donor (often a close relative) give a part of their liver for transplant. This can be successful, but it carries risks for the donor.
- Another option is to treat the patient first with chemotherapy and radiation. This is followed by a transplant when a liver becomes available. This has been done as part of a clinical trial in the past, and may become a standard treatment for perihilar bile duct cancer in the future.
Possible risks and side effects: Like other surgeries for bile duct cancer, a liver transplant is a major operation with potential risks (bleeding, infection, complications from anesthesia, etc.). But there are also some additional risks after this surgery. People who get a liver transplant have to be given drugs to help suppress their immune system and prevent them from rejecting the new organ. These drugs have their own risks and side effects, especially the risk of getting serious infections. Some of the drugs used to prevent rejection can also cause high blood pressure, high cholesterol, and diabetes, can weaken the bones and kidneys, and can lead to the development of another cancer. After a liver transplant, regular blood tests are important to check for signs of rejection. Sometimes liver biopsies are also taken to see if rejection is occurring and if the anti-rejection medicines need to be changed.
B. Palliative surgery:
This may be performed to relieve symptoms or treat (or even prevent) complications, such as blockage of the bile ducts. This type of surgery is performed when the tumor is too widespread to be completely removed. Palliative surgery is not expected to cure the cancer, but it can sometimes help someone feel better and sometimes can even help them live longer. Palliative surgery includes biliary bypass or inserting biliary stent
- Biliary bypass: In some cases, a doctor may think that a cancer is resectable based on the information available (imaging tests, laparoscopy, etc.), but once surgery is started it becomes clear that the cancer is too advanced to be removed completely. At this point the surgeon may do a biliary bypass to allow the bile to flow into the intestines to reduce symptoms such as jaundice or itching. In this palliative procedure, the surgeon creates a bypass around the tumor blocking the bile duct by connecting part of the bile duct before the blockage with a part of the duct that lies past the blockage. Often, the gallbladder is used to provide some of the bypass.
- Biliary stent or biliary catheter: If cancer is blocking the bile duct, the doctor may insert a small tube (called a stentor catheter) into the duct to help keep it open. This may be done as part of a cholangiography procedure such as percutaneous transhepatic cholangiography (PTC) or endoscopic retrograde cholangio-pancreatography (ERCP) or, in some cases, during surgery. A stent opens the duct to allow the bile to drain into the small intestine, while a catheter drains into a bag outside the body that can be emptied when needed. The stent or catheter may need to be replaced every few months if it becomes clogged and to reduce the risk of infection and gallbladder inflammation.
Adapted in part from “Liver Surgical patients information sheet” The Virginia Mason Seattle Medical Center, Seattle, WA, USA.
This is a treatment with high-energy rays or particles that destroy cancer cells.
Timing of Radiation Therapy:
- Adjuvant therapy is treatment after surgery for resectable cholangiocarcinoma. It is meant to kill any deposits of cancer cells that remain after surgery, but are too small to see. Some doctors believe adjuvant radiation therapy is helpful, but more research is needed.
- Neoadjuvant therapy is a treatment before surgery for borderline resectable cholangiocarcinoma. Doctors may use radiation therapy before surgery for cancers that are thought to be resectable. This is done to try to shrink the cancer and make the operation easier. It’s not clear how helpful this is for cholangiocarcinoma.
- Chemoradiation is a therapy for some advanced cholangiocarcinomas. Radiation therapy can also be used as a therapy for patients whose cancer has not spread widely throughout the body but is not resectable. While treatment in this case does not offer a cure, it may help patients to live longer. Radiation therapy may be given along with chemotherapy to help it work better. This is called chemoradiation. Most often, the chemo drugs used are 5-fluorouracil (5-FU) or capecitabine (Xeloda®). The main drawback of this approach is that the side effects tend to be worse than giving radiation alone.
- Palliative therapy using radiation is often used to palliate (relieve) symptoms when a patient’s cancer is too advanced to be cured. It may be used to relieve pain or other symptoms by shrinking tumors that block the passage of blood or bile, or press on nerves.
Radiation Therapy Types:
There are 2 main types of radiation therapy either external beam radiation and brachytherapy (internal radiation therapy).
- External beam radiation therapy (EBRT): This type of radiation therapy uses x-rays from a machine outside the patient’s body to kill cancer cells. It is the most common form of radiation therapy for cholangiocarcinoma. The treatment is much like getting an x-ray, but the radiation is more intense.The procedure itself is painless. Before your treatments start, the radiation team will take careful measurements to determine the correct angles for aiming the radiation beams and the proper dose of radiation. Each treatment lasts only a few minutes, but the setup time — getting you into place for treatment — usually takes longer. Most often, radiation treatments are given 5 days a week for several weeks.Side effects from radiation often start 1-2 weeks after starting treatment, and usually get better over time once treatment is over. These side effects may include skin changes, ranging from redness to blistering and peeling (in the area being treated), nausea and vomiting, diarrhea, fatigue (tiredness), hair loss (on the skin in the area being treated), low blood cell counts, and liver damage. EBRT can be given using various machines:
- Three-dimensional conformal radiation therapy (3D-CRT) uses special computers to precisely map the location of the tumor(s). Radiation beams are shaped and aimed at the tumor(s) from several directions, which makes it less likely to damage normal tissues. Most doctors now recommend using some form of 3D-CRT when it is available.
- Intensity-modulated radiation therapy (IMRT) is an advanced form of 3D therapy. It uses a computer-driven machine that actually moves around the patient as it delivers radiation. In addition to shaping the beams and aiming them at the bile duct from several angles, the intensity (strength) of the beams can be adjusted to minimize the dose reaching the most sensitive normal tissues. This lets doctors deliver an even higher dose to the cancer areas. This procedure is available in many major hospitals and cancer centers.
- Stereotactic body radiotherapy (SBRT) uses the techniques of 3D-CRT and IMRT, but gives the radiation over fewer sessions. A course of SBRT may take less than a week, while a course of radiation using these other techniques often takes place over 3 to 6 weeks.
- Brachytherapy: This may be known as intrabiliary brachytherapy. This type of treatment uses small pellets of radioactive material placed next to or directly into the cancer. The radiation travels a very short distance, so it affects the cancer without causing much harm to nearby healthy body tissues. Brachytherapy is sometimes used in treating people with cholangiocarcinoma by placing the pellets in a tube, which is inserted into the bile duct for a short time. It can be used alone, or along with EBRT. At this time, it’s mostly used as a palliative treatment.
Interventional Radiologist are responsible for treating patients with various loco-regional therapy approaches which include:
- Percutaneous treatment approach e.g. radiofrequency, cryotherapy
- Trans-arterial treatment approach e.g. trans-arterial chemoembolization (TACE), Y90 tarns-arterial radioembolization, hepatic artery infusion (HAI)
- Endoscopic treatment approach e.g photodynamic therapy (PDT)
A. Radiofrequency Ablation
- For inoperable liver tumors, radiofrequency ablation (RFA) offers a nonsurgical, localized treatment that kills the tumor cells with heat, while sparing the healthy liver tissue. Thus, this treatment is much easier on the patient than systemic therapy. Radiofrequency energy can be given without affecting the patient’s overall health and most people can resume their usual activities in a few days.
- In this procedure, the interventional radiologist guides a small needle through the skin into the tumor. From the tip of the needle, radiofrequency energy (similar to microwaves) is transmitted to the tip of the needle, where it produces heat in the tissues. The dead tumor tissue shrinks and slowly forms a scar. The FDA has approved RFA for the treatment of liver tumors.
- In a small number of cases, RFA can extend patients’ lives, but it is generally palliative. Depending on the size of the tumor, RFA can shrink or kill the tumor, extending the patient’s survival time and greatly improving their quality of life while living with cancer.
- Because it is a local treatment that does not harm healthy tissue, the treatment can be repeated as often as needed to keep patients comfortable. It is a very safe procedure, with complication rates on the order of two to three percent, and has been available since the late 1990s.
- By decreasing the size of a large mass, or treating new tumors in the liver as they arise, the pain and other debilitating symptoms caused by the tumors are relieved. While the tumors themselves may not be painful, when they press against nerves or interfere with vital organs, they can cause pain. RFA is effective for small to medium-sized tumors and emerging new technologies should allow the treatment of larger cancers in the future. Radiofrequency advantages include
- Effective when all the cancer is localized in the liver
- Can be used to treat primary liver cancer and tumors that have metastasized (spread) from other areas in the body to the liver
- Usually does not require general anesthesia
- Well tolerated so most patients can resume their normal routine the next day and may feel tired for a few days
- Can be repeated if necessary
- May be combined with other treatment options
- Can relieve pain and suffering for many cancer patients
B. Cryoablation
Cryoablation is similar to RFA in that the energy is delivered directly into the tumor by a probe that is inserted through the skin. But rather than killing the tumor with heat, cryoablation uses an extremely cold gas to freeze it. This technique has been used for many years by surgeons in the operating room, but in the last few years, the needles have become small enough to be used by interventional radiologists through a small nick in the skin, without the need for an operation. The “ice ball” that is created around the needle grows in size and destroys the frozen tumor cells.
C. Trans-arterial chemoembolization (TACE):
- Chemoembolization is a minimally invasive treatment for liver cancer that can be used when there is too much tumor to treat with radiofrequency ablation (RFA), when the tumor is in a location that cannot be treated with RFA, or in combination with RFA or other treatments.
- Chemoembolization delivers a high dose of cancer-killing drug (chemotherapy) directly to the organ while depriving the tumor of its blood supply by blocking, or embolizing, the arteries feeding the tumor. Using imaging for guidance, the interventional radiologist threads a tiny catheter up the femoral artery in the groin into the blood vessels supplying the liver tumor. The embolic agents keep the chemotherapy drug in the tumor by blocking the flow to other areas of the body. This allows for a higher dose of chemotherapy drug to be used, because less of the drug is able to circulate to the healthy cells in the body.
- Chemoembolization usually involves a hospital stay of two to four days.
- Patients typically have lower than normal energy levels for about a month afterwards.
- Chemoembolization is a palliative, not a curative, treatment. It can be extremely effective in treating primary liver cancers, especially when combined with other therapies. Chemoembolization has shown promising early results with some types of metastatic tumors.
- Although the individual materials used in this treatment are FDA approved, the treatment itself is not approved for intra-arterial therapy of liver tumors.
D. Yttrium-90 Trans-arterial Radioembolization
- Radioembolization is very similar to chemoembolization but with the use of radioactive microspheres. This therapy is used to treat both primary and metastatic liver tumors.
- This treatment incorporates the radioactive isotope Yttrium-90 into the embolic spheres to deliver radiation directly to the tumor. Each sphere is about the size of five red blood cells in width. These beads are injected through a catheter from the groin into the liver artery supplying the tumor. The beads become lodged within the tumor vessels where they exert their local radiation that causes cell death. This technique allows for a higher, local dose of radiation to be used, without subjecting healthy tissue in the body to the radiation. The Yttrium-90 radiates from within and, since it is administered in the hepatic artery, it can be viewed as “internal” radiation.
- Radioembolization is a palliative, not a curative, treatment-but patients benefit by extending their lives and improving their quality of life. It is a relatively new therapy that has been effective in treating primary and metastatic liver cancers.
- It is performed as an outpatient treatment. There are fewer side effects from this treatment compared to standard cancer treatments, with the main one being fatigue for seven to 10 days.
E. Hepatic Artery Infusion (HAI):
- Hepatic Artery Infusion (HAI) therapy delivers medicine (chemotherapy) directly to the liver through the hepatic artery. Compared to traditional (systemic) chemotherapy, this allows the drug to reach the tumors in the liver at a higher concentration, without causing additional side effects to the rest of the body.
- The drug is delivered from a pump that is implanted (placed by surgery) just below the skin, in the abdomen, and connects to the blood vessel that supplies the liver. The pump is powered by the patient’s body heat.
- The hepatic artery supplies blood to most bile duct tumors in the liver. The healthy parts of the liver can remove most of the remaining drug before it can reach the rest of the body.
- HAI therapy is used to treat intrahepatic cholangiocarcinoma. If disease has spread significantly beyond the liver, HAI therapy may not be an option.
- Research shows that HAI may allow some people whose cancer was not removable by surgery to live longer.1,2,3 A study published in 2024 showed over 30% of patients with unresectable intrahepatic cholangiocarcinoma treated with HAI and systemic chemotherapy survived for at least three years.2 Patients wishing to be treated with this technique must be able to tolerate surgery under general anesthesia to implant the pump and insert a catheter into the hepatic artery.
- The drug used in HAI to treat cholangiocarcinoma is floxuridine. The pump is refilled every two weeks, alternating between floxuridine and heparinized saline. When active treatment is completed, the pump may be maintained with glycerin to extend the time between refills.
1Cercek A et al. JAMA Oncol. 2020;6(1):60-67.
2Franssen S et al. Ann Surg Oncol. 2024;31(1):115-124.
3Holster J et al. Ann Surg Oncol. 2022;29(9):5528-5538.
The Intera 3000 Hepatic Artery Infusion Pump is indicated for the continuous arterial administration of JND Therapeutics Floxuridine for Injection, USP, heparinized saline, and glycerin. The approved labeling for JND Therapeutics Floxuridine for Injection, USP stipulates the indications, contraindications, and warnings for use of the drug in the pump. The Intera 3000 Hepatic Artery Infusion Pump is contraindicated for use in patients with extensive extrahepatic disease or limited hepatic function. Possible adverse events of the pump are those potential risks associated with any implanted drug delivery device and include: catheter thrombosis, bolus path occlusion, vessel thrombosis, pump dislodgement, seroma, or recurrent hematoma, infection, extravasation, catheter shear, dislodgement or leakage, migration, arterial pseudoaneurysm, arterial dissection, and extrahepatic perfusion.
Caution: Federal law (USA) restricts this device to sale by or on the order of a physician. Please review the full safety information at https://www.interaoncology.com/patients-caregivers/hai-therapy/safety-information.
F. Photodynamic therapy (PDT)
For this technique, a light-activated drug is injected into a vein. A few days later, an endoscope (a long, flexible tube that can be used to look inside the body) is passed down the throat and into the bile duct. A special red light on the end of the endoscope is aimed at the tumor, causing the cells to die. The combination of PDT and stenting can help patients with cholangiocarcinoma whose tumors aren’t resectable live longer.
G. Histotripsy
Histotripsy, also known as tissue disruption therapy, is a novel medical technique involving the precise destruction of targeted tissues using focused ultrasound waves.
Histotripsy is a treatment option that doesn’t involve surgery. It uses sound waves to create tiny bubbles in tissues, breaking them down without any cuts, so anesthesia is unnecessary.
This technology shows promise in treating various medical conditions, including benign and malignant tumors, without causing significant collateral damage to surrounding healthy tissue. Histotripsy offers potential benefits such as reduced recovery times, minimized risks, and improved patient outcomes in various therapeutic applications.
Experience with histotripsy is still early, effectiveness and safety have been studied in the #HOPE4LIVER Trials.
The FDA has approved histotripsy for the treatment of unresectable liver tumors, including cholangiocarcinoma.
Chemotherapy (chemo) is anti-cancer drugs given through a vein or by mouth. These drugs enter the bloodstream and reach all areas of your body, making this treatment useful in some cancers that have spread to organs beyond the bile ducts. Because the drugs reach all the areas of the body, this is known as a systemic treatment.
Unfortunately, chemo has not been very effective against bile duct cancer, so its use has been somewhat limited. Uses of chemotherapy include:
- Neoadjuvant chemotherapy is given before surgery for borderline resectable cancer or while waiting for a liver transplantation.
- Adjuvant chemotherapy happens after surgery for resectable cancers. Chemotherapy may be used after surgery (often along with radiation therapy) to try to lower the risk of the cancer returning. This is known as adjuvant chemotherapy if given alone or adjuvant chemoradiotherapy if given along with radiation therapy.
- Palliative therapy chemo can help shrink tumors or slow their growth for a time. This can help relieve symptoms from the cancer, for instance, by shrinking tumors that are pressing on nerves and causing pain.
- Before liver transplantation, chemotherapy may be used to keep bile duct cancer under control while waiting for a liver transplant.
Doctors give chemo in cycles, with each period of treatment followed by a rest period to give your body time to recover. Chemo cycles generally last about 3 to 4 weeks. Chemo is often not recommended if you are in poor health, but advanced age by itself is not a barrier to getting chemotherapy.
Chemo drugs work by attacking and killing cancer cells in your body that are dividing quickly. However, other cells in your body, such as those in the bone marrow, the lining of the mouth and intestines, and hair follicles, also divide quickly. These cells can be affected by chemo, which can lead to side effects. The side effects of chemo depend on the type and dose of drugs given and the length of time they are taken. These side effects can include:
- Hair loss
- Mouth sores
- Loss of appetite
- Nausea and vomiting
- Nerve damage (neuropathy), which can lead to trouble swallowing or numbness, tingling, and even pain in the hands and feet
- Increased chance of infections (due to low white blood cell counts)
- Easy bruising or bleeding (due to low blood platelet counts)
- Fatigue (due to low red blood cell counts)
These side effects are usually short-term and go away after treatment is finished. There are often ways to lessen these side effects. For example, drugs can be given to help prevent or reduce nausea and vomiting. Be sure to ask your doctor or nurse about medicine to help reduce side effects, and let him or her know when you do have side effects so they can be managed effectively.
Learn More about being prescribed 5-FU
or Capecitabine (Xeloda)
As researchers have learned more about the gene and protein changes in cells that cause cancer, they’ve developed newer drugs known as Targeted Therapy to specifically target these changes. Targeted therapies more precisely identify and attack cancer cells when compared to chemotherapy. They sometimes work when standard chemo drugs don’t, and they often have different (and less severe) side effects. They can be used either along with chemo or by themselves. Targeted therapy is used to treat many different kinds of cancer. These drugs are being researched to see if they can help treat cholangiocarcinoma.
Three drugs have been approved by the Food and Drug administration (FDA) for cholangiocarcinoma including:
- Pemigatinib (Pemazyre)
- Ivosidenib (Tibsovo) for cholangiocarcinoma with IDH1 mutation
- LYTGOBI (futibatinib)
Many other targeted therapy drugs are available to patients through clinical trials.
Immunotherapy is treatment that helps a person’s immune system better recognize and destroy cancer cells. Immunotherapy can encourage your immune system to attack cancer cells. Immunotherapy may have side effects and you should discuss your options with your physician to understand how and if immunotherapy would be a treatment option for you.
For up to date information on immunotherapy, visit The American Cancer Society’s Page on Immunotherapy.
If you have a high tumor mutation burden, high levels of microsatellite instability (MSI-H) or mismatch repair deficiency (dMMR), you should consider immunotherapy as a possible treatment. Microsatellite instability and mismatch repair deficiency are types of genetic changes to a cell that interfere with its ability to repair itself. This can lead to cancer cells that are very different from normal cells, which can make them more “visible” to the body’s immune system.
Immunobiology of Cholangiocarcinoma
FDA grants accelerated approval to pembrolizumab for first tissue/site agnostic indication
This is treatment given to help control or reduce symptoms caused by advanced cholangiocarcinoma. It is not meant to be a curative treatment. If your cancer has spread too far to be completely removed by surgery, doctors may focus on palliative surgery or palliative radiotherapy, as well as other palliative symptomatic therapies. Because these cancers tend to advance quickly, doctors try to use palliative therapies that are less likely to affect your quality of life, when possible.
- Pain: Control of pain is one of the most important aspects of cancer care. Pain not only affects quality of life and ability to function, it may also lower your tolerance for needed cancer treatments. For many cancer patients, pain results from the spread of the tumor into surrounding nerves and other tissues. In cholangiocarcinoma, to treat the pain, interventional radiologists insert catheters or needles into nerves that convey sensations of pain from the bile duct and intestinal area to the brain by injecting these nerves with alcohol or other agents that destroy the nerves causing the pain. This can be done under CT guidance.
A particularly painful complication of cancer is when the disease spreads (metastasizes) to bones. In a technique called transcatheter embolization, interventional radiologists inject tiny particles, the size of grains of sand, through a catheter and into the artery that supplies blood to the tumor. The particles cause clotting that decreases the tumor’s blood supply, reducing pain and decreasing the likelihood of bone fracture.
- Bleeding: If a cancer spreads to the blood vessels it may cause hemorrhage or bleeding. An interventional radiology technique called transcatheter embolization can be used to clot the affected blood vessels and stop the bleeding.
- Organ Obstruction and Infection: Cancers can obstruct the normal flow of urine or bile, causing these fluids to build up in the body. If left untreated, these conditions are not only painful but may also result in organ failure or infection. Under X-ray guidance, catheters can be inserted to drain the collection of fluids. Often, a small device called a stent is inserted into the organ to bypass the obstruction and allow fluids to drain internally.
- Blood Clots: One common side effect of cancer or cancer treatments is the development of blood clots, or emboli, that can be life-threatening if they travel to the brain, lungs or heart. There are two interventional radiology procedures that can reduce the risks posed by blood clots:
- Intra-arterial thrombolysis. In this technique, the interventional radiologist guides a catheter through the blood vessels and to the site of a blood clot. Clot-busting drugs are infused through the catheter to break up the clot.
- Filter placement. This technique is most often used when a blood clot is detected in the blood vessels of the leg (a condition called deep vein thrombosis). The interventional radiologist guides a small filter into the blood vessel that receive blood from the lower body (the vena cava) and carries it to the heart. If the blood clot dislodges from the vein in the leg, the filter will trap it before it can reach the heart.