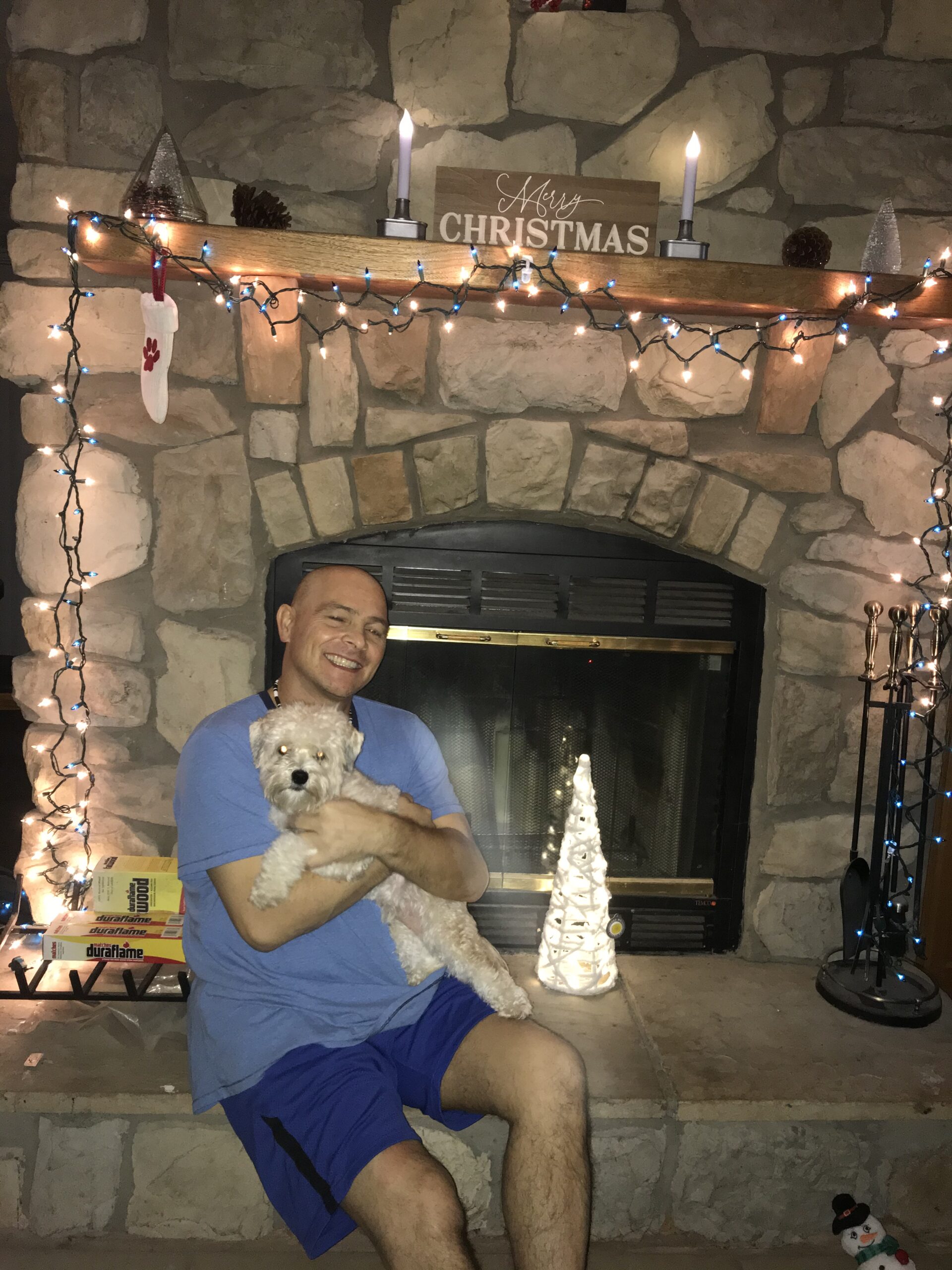
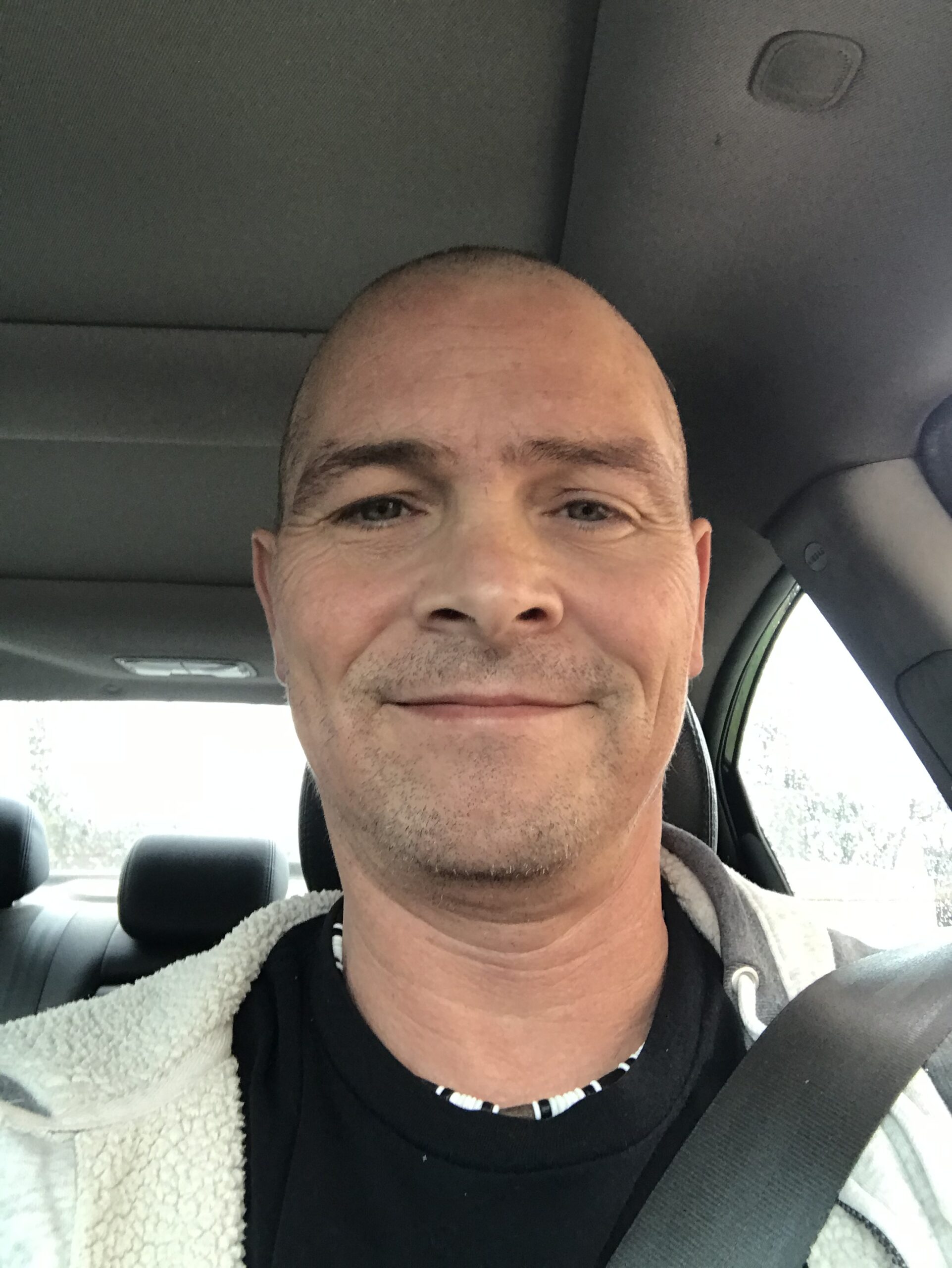
Long-Term Survivor Stories - Robert Bickel
Working out was something of a side-hustle for me the last three years. I used it as motivation to quit smoking and set the stage for the next chapter of my life. With two daughters in college that were not too far off-major milestones and such. Despite that vice, I maintained a fairly healthy lifestyle and was quite content with my relative position at the gym amongst the others. So, when COVID-19 hit in March 2020 you can imagine my disappointment when the gym closed its doors. For three months I toiled at home ever mindful that I needed to stay engaged physically and mentally to manage my program.
In June 2020, the gym reopened, albeit with a bit of a different feel. It was a pretty desolate place in fact. So, at about three weeks post opening, I developed a slight, but somewhat uncomfortable feeling (or dull pain) in the upper right area of my abdomen. I let this dull pain continue for a couple of weeks rationalizing that it was something related to a new exercise or strain at the gym. After all, I had been out of commission for three months.
Finally, after another few weeks, I made an appointment with my GP. He and I discussed this relatively minor ache but felt it important enough-and symptomatically in close proximity to a few dangerous areas- that we should investigate it further. He ordered an ultrasound but the results of this were not overly conclusive. He did stipulate that I may be having a gallbladder surgery at some point though. In the meantime, I had promised my daughters a family trip, so my focus was on the prospects of getting away, dull pain notwithstanding. My first inclination that something was a bit off was while away from home. My eyes began to jaundice and while it was certainly an uneasy feeling and sight, I maintained my enthusiasm for the vacation we were on.
MY DIAGNOSIS & TREATMENT
When I saw my doctor after returning home, he referred me off to a gastroenterologist. We suspected a blockage but obviously needed confirmation. We also suspected that I may need to have my gallbladder removed so we sent all the requisite info off. Just as we were scheduling who would do this probable surgery the specialist called and after having looked at my ultrasound results asked for me to get a CT scan. This is the moment I knew something was not right and the pit of my stomach turned. I subsequently had an ERCP stent put in my bile duct as they were able to see it was blocked by a mass of approximately 2 cm. They did not know, however, if it was cancerous but took a biopsy and promised me that I would know within a day or so.
On August 11, 2020, I was told I had a cancerous mass. I was immediately referred to Indiana University for a Whipple Surgery (Dr. Michael House) – who I was told was one of the best in the business. I was fairly relieved at this designation so I resigned myself to the fact that I had a small cancerous mass that could be surgically removed by a ringer. After all, the mass didn’t look overly impressive from a size standpoint, so I was good with that.
In late September I had Whipple surgery. I was told beforehand what the procedure entailed of course. They would ideally go in and get the cancerous mass and hopefully, that would be it. No chemo–just follow-up thereafter. I was confident in the doctor and my hope was restored.
The day of the surgery came, and I was not surprisingly nervous. I had this cloud of anxiety and uncertainty that I couldn’t escape. I understood the surgery to be very involved but that didn’t concern me so much. It was the thought of: “What if?” That’s it.
In some cases, a Whipple surgery must be aborted because the cancer has been found to have metastasized. I was unfortunately one such case. The 2 cm mass and its cancerous cells had traveled up to my liver–albeit in such small presentations they couldn’t even see them on the CT scan. It was only discovered during the surgery through feeling in the liver.
AFTER MY SURGERY
After my surgery, but while I was in recovery, the doctor called my oldest daughter to give her an update–the news if you will. I will forever feel terrible that she had to take this call. Up until this call, the hardest thing she had to deal with was One Direction splitting up. Imagine being on the receiving end of a phone call–with the prior understanding that all will be well, or at least hopeful–and being told that your father has Stage 4 cancer. I try not to anymore.
During my hospital stay, Dr. House informed me that I would have a great chance at being involved in clinical trials for treatment. It didn’t occur to him that this was not on my list of preferred outcomes pre- or post-op. He was a steadying and compassionate resource, nonetheless. I recall looking this poor man in the eyes every day until he discharged me asking him if he thought I stood a chance at beating this with the chemo and trials. He had taken the time to get to know me and with that knowledge said if anyone could, it would be you. I’ll never forget his presence and the power of that affirmation at that moment.
Discharged, my next step was to simply heal so we could tackle chemo right away. The obvious thought was to get in there and kill it (as Dr. House would say) as soon as we could. It would be a little more than three weeks post-op that I began chemo on a clinical trial. I did this in combination with a standard of care. My oncologist, Dr. Anita Turk, understood who I was from our first meeting. I would not be defeated and would do whatever it took to beat this. In another life, I had defeated a terrible malady and I explained to the doctor where my mind was: this will not be the toughest fight of my life, rest assured I have fought that and continue to daily. I will use everything I have learned along the way and trust in God to guide me.
We started the chemo in October. I was anxious about side effects and hoped that they would be minimal. I was especially concerned about my physical appearance. Yet I accepted my lot like so many brave people do in this position. This is what I have to do now.
MY JOURNEY CONTINUES
Every two months I was given an update through CT scan and labs. My tumor markers had retracted from 7,000+ to a normal 6. A 99.9% improvement. The lesions on my liver were “inconspicuously absent”. The journey had lasted six months so far and I was making “amazing” and “stellar” progress until I showed some disease progression in a few lymph nodes. So, I was removed from the trial. However, I was told they were going to have to remove me anyway because they were so aggressive with my treatment and the toxicity would demand it. Despite the minor setback, I was ecstatic at my recovery.
Early on I read on the CCF website that when diagnosed with cancer such as this, the most important thing you can do is get a second opinion. So, with some curiosity, and in combination with the rarity of this diagnosis and my progress I asked myself, how could anyone have all the answers? So, I asked to have my records forwarded to Mayo Clinic for feedback on what they thought about further treatment options. And I do think it’s important to note that I did this not because I was in any way disappointed with my current team. I’m glad I did. The doctors there confirmed we were on the right track and even commented that my recovery was pretty impressive and that you (or they) don’t often see the kind of response I was blessed with. Just about a CR (complete response).
MY POST-DIAGNOSIS
I am now one plus year post-diagnosis. There are certain cancer survivors with our cancer that have managed to overcome and be blessed with a recovery measured in years and not months. I know they understand how fortunate they are. But such is the somber truth of a rare disease: Is it lethal because it’s unknown, or is it just vicious? I happen to think it’s a matter of the unknown and the amount of research developed. God bless those involved. I absolutely believe that with the resources being poured into this research we are headed for exciting times.
As I contemplate all of this, I realize in the meantime I–we–must continue to avail ourselves to the trials in the hope that this might just be the time or the one. We must continue to look not so much into the future and measure our war chest on lengthy battles–rather the only thing I have to do is be the best and strongest version of me today–willing to go just one more step at the gym or park, take one more minute to meditate or pray, and thank God for the day he has given me. The key for me is understanding that I don’t have to win the rest of my life, today. I only have to try to win today. And if I do, that by simply suiting up and getting involved in my own treatment I will be well-positioned for tomorrow.